Mantle cell lymphoma (MCL) is a rare and aggressive B-cell lymphoma1
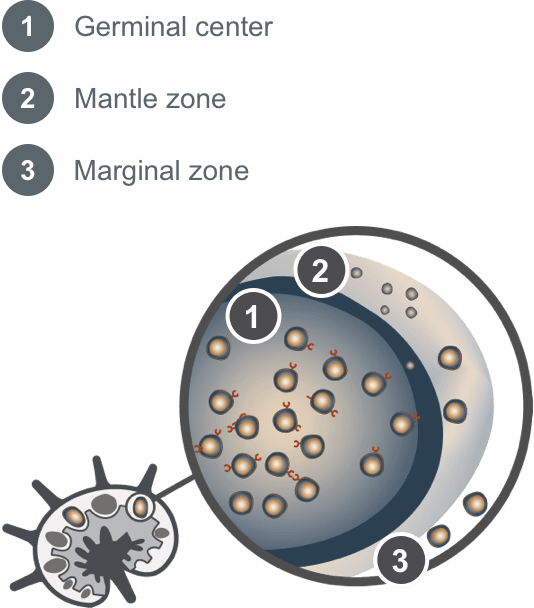
MCL develops from malignant B cells within the lymph node2-5
- Originates in the mantle zone of lymphoid follicles3,5
- MCL cells characteristically exhibit chromosomal translocation t(11;14) (q13;q32) and overexpression of cyclin D1 in addition to expression of the CD19 and CD20 antigens4,6,7
- Cyclin D1 disrupts the cell cycle, which results in MCL oncogenesis4

Pinch to zoom
Adapted from Swerdlow SH, Campo E, Pileri SA, et al. Blood. 2016;127(20):2375-2390 and Arruga F, Vaisitti T, Deaglio S. Front Oncol. 2018;8:550. doi:10.3389/fonc.2018.00550
MCL cells are often located in the peripheral blood, bone marrow, spleen, and gastrointestinal tract8
Patient demographics9,10
- Median age is 69
- ~3x more common in males
- Non-Hispanic, White
Most patients present with generalized lymphadenopathy; additional signs and symptoms of MCL include11-15:
- Unexplained weight loss
- Drenching night sweats
- Fever
- Fatigue
- Lymphocytosis
- Pain
- Hepatosplenomegaly
- GI symptoms
- Skin rash
Pathological tests used for MCL diagnosis and risk assessment1
IHC stains and flow cytometry
- Cyclin D1
- Ki-67 proliferation index
- CD19
- CD20
- CD5
- CD23
Genetic testing/chromosomal evaluation
- TP53
- IGHV status
- FISH test for t(11;14)
Diagnostic testing
- PET and CT scans
- Bone marrow biopsy
- CBC, blood chemistry, and LDH
Other testing
- Colonoscopy
- Upper GI endoscopy
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas recommend including TP53 sequencing and Ki-67 immunohistochemistry as an essential component of diagnostic testing for MCL1
CD20, CD3, CD5, cyclin D1, CD10, CD21, CD23, BCL2, BCL6, and SOX11 are also recommended as essential components of the diagnostic immunohistochemistry panel1
NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way.
MCL characteristics associated with high-risk for aggressive disease5,16
- Presence of the TP53 mutation
- Ki-67 index >30%
- Blastoid/pleomorphic MCL
- Complex karyotype
- Presence of B symptoms
- Elevated LDH
- High-risk MIPI score
CBC=complete blood count; CD=cluster of differentiation; CT=computed tomography; FISH=fluorescence in situ hybridization; GI=gastrointestinal; IGHV=immunoglobulin heavy chain variable; IHC=immunohistochemistry; LDH=lactate dehydrogenase; MCL=mantle cell lymphoma; MIPI=Mantle Cell Lymphoma International Prognostic Index; NCCN=National Comprehensive Cancer Network® (NCCN®); PET=positron emission tomography.
References: 1. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas. V.2.2025. © National Comprehensive Cancer Network, Inc. 2025. All rights reserved. Accessed February 12, 2025. To view the most recent and complete version of the guideline, go online to NCCN.org. 2. Arruga F, Vaisitti T, Deaglio S. The NOTCH pathway and its mutations in mature B cell malignancies. Front Oncol. 2018;8:550. doi:10.3389/fonc.2018.00550 3. Weisenburger DD, Kim H, Rappaport H. Mantle-zone lymphoma: a follicular variant of intermediate lymphocytic lymphoma. Cancer. 1982;49(7):1429-1438. 4. Pileri SA, Falini B. Mantle cell lymphoma. Haematologica. 2009;94(11):1488-1492. 5. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375-2390. 6. Aguilera NS, Bijwaard KE, Duncan B, et al. Differential expression of cyclin D1 in mantle cell lymphoma and other non-Hodgkin’s lymphomas. Am J Pathol. 1998;153(6):1969-1976. 7. Dreyling M, on behalf of the European MCL Network. Mantle cell lymphoma: biology, clinical presentation, and therapeutic approaches. Am Soc Clin Oncol Educ Book. 2014;34:191-198. 8. Veloza L, Ribera-Cortada I, Campo E. Mantle cell lymphoma pathology update in the 2016 WHO classification. Ann Lymphoma. 2019;3(3):1-17. 9. Fu S, Wang M, Lairson DR, Li R, Zhao B, and Du XL. Trends and variations in mantle cell lymphoma incidence from 1995 to 2013: A comparative study between Texas and National SEER areas. Oncotarget. 2017;8(68):112516-112529. 10. Fu S, Wang M, Li R, Lairson DR, Zhao B, and Du XL. Increase in survival for patients with mantle cell lymphoma in the era of novel agents in 1995–2013: findings from Texas and national SEER areas. Cancer Epidemiol. 2019;58:89-97. 11. Carvajal-Cuenca A, Sua LF, Silva NM, et al. In situ mantle cell lymphoma: clinical implications of an incidental finding with indolent clinical behavior. Haematologica. 2012;97(2):270-278. 12. Inamdar AA, Goy A, Ayoub NM, et al. Mantle cell lymphoma in the era of precision medicine-diagnosis, biomarkers and therapeutic agents. Oncotarget. 2016;7(30):48692-48731. 13. National Cancer Institute. Mantle cell lymphoma. National Cancer Institute surveillance, epidemiology, and end results program website. https://seer.cancer.gov/seertools/hemelymph/51f6cf57e3e27c3994bd5357/ Accessed December 1, 2024. 14. Wang Y, Ma S. Risk factors for etiology and prognosis of mantle cell lymphoma. Expert Rev Hematol. 2014;7(2):233-243. 15. Romaguera JE, Medeiros LJ, Hagemeister FB, et al. Frequency of gastrointestinal involvement and its clinical significance in mantle cell lymphoma. Cancer. 2003;97(3):586-591. 16. Cohen JB, Zain JM, Kahl BS. Current approaches to mantle cell lymphoma: diagnosis, prognosis, and therapies. Am Soc Clin Oncol Educ Book. 2017;37:512-525. 17. Visco C, Tisi MC, Evangelista A, et al. Time to progression of mantle cell lymphoma after high-dose cytarabine-based regimens defines patients risk for death. Br J Haematol. 2019;185(5):940-944. 18. Bond DA, Switchenko JM, Villa D, et al. Early relapse identifies MCL patients with inferior survival after intensive or less intensive frontline therapy. Blood Adv. 2021;5(23):5179-5189.